Conference Summaries
Glycaemic variability and diabetic complications
Presented by:Antonio Ceriello, MD
Institut d'Investigacions Biomèdiques August Pi I Sunyer (IDIBAPS), Barcelona, Spain; Dept. of Cardiovascular and Metabolic Diseases, IRCCS Multimedica, Milan, Italy
Glycaemic variability is an integral component of glucose homoeostasis, and in recent years has become one of the ‘hot topics’ in type 2 diabetes, as shown by the ever increasing number of publications on the subject1. Although it has not yet been definitively confirmed as an independent risk factor for diabetes-associated complications, glycaemic variability can represent the presence of excess glycaemic excursions and, consequently, the risk of hyperglycaemia or hypoglycaemia.
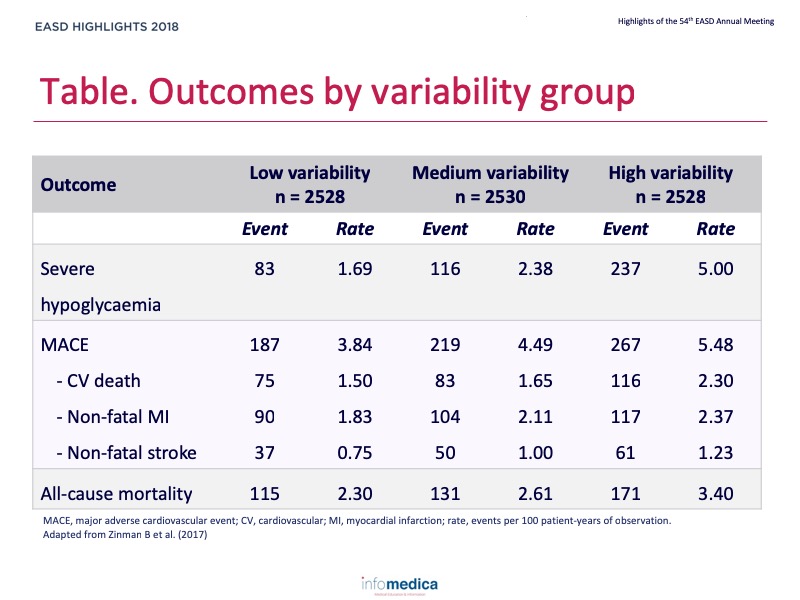
The first key historical study, with over 10 years of follow-up, showing that fasting glucose variability was an independent predictor of cardiovascular mortality, was published almost 20 years ago2. Considering data from clinical studies where treatment may be more intense than in real-life settings, the ADVANCE trial reported that the consistency of glycaemic control was important in order to reduce the risks of both macrovascular and microvascular events3. More recently, DEVOTE 2 showed that higher day-to-day fasting glycaemic variability was associated with increased risk of severe hypoglycaemia and all-cause mortality (Table)4. Lastly, the latest analysis of the VADT trial further documented that variability of fasting glucose plays a role in the development of cardiovascular complications, beyond the influence of standard fasting glucose measures; the adverse consequences of fasting glucose variability on cardiovascular disease appear to be highest in patients receiving intensive glucose control5. Considering these and other studies, the link between glucose variability and diabetic complications, and especially increased cardiovascular risk, is well documented.
Oxidative stress, in particular the increased superoxide production at the mitochondrial level, has been suggested as a key link between hyperglycaemia and diabetic complications6. Markers of oxidative stress, such as nitrotyrosine, are indeed increased by oscillating levels of glucose. In vitro, after exposure of cells to constant high glucose the antioxidant enzymes SOD-1 and GPx-1 are increased, while in oscillating glucose conditions SOD-1 is increased and GPx-1 is not: SOD-2 and catalase remain unchanged under both conditions7. The dysregulation of endogenous GPx-1 under these conditions has been linked to critical involvement of miR-185, which is upregulated by oscillating glucose levels. These observations also help to explain why glucose oscillations may exert more deleterious effects on the endothelium than high glucose levels. The damage to cells is not because more free radicals are produced during glucose oscillations, but rather because cells are less capable of counteracting the deleterious effects of free radicals. This assumption has been confirmed through studies on human subjects where recovery from hypoglycaemia worsens endothelial function and increases oxidative stress in both healthy control subjects and individuals with type 1 diabetes8.
There are now good opportunities for clinical monitoring and use of markers for glycaemic variability. In 2017, international consensus was established for the use of continuous glucose monitoring (CGM)9. CGM, either from real-time use (rtCGM) or intermittently viewed (iCGM), addresses many of the limitations inherent in HbA1c testing and self-monitoring of blood glucose. In particular, the consensus panel recommended that CGM data should be used to assess hypoglycaemia and glucose variability. Moreover, stable glucose levels are defined as a coefficient of variation (CV) of <36%, and unstable glucose levels should be defined as a CV ≥36%. CV should be considered as the primary measure of glycaemic variability.
Key messages / Clinical perspectives
- Glycaemic variability is an integral component of glucose homeostasis, although it is not fully endorsed as an independent risk factor for the onset of long-term diabetic complications.
- However, the relationship between glycaemic variability and the risk of severe hypoglycaemia is well established.
- The relationship between glycaemic variability and diabetes-related complications is clearly evident.
- A number of pharmacological and non-pharmacological therapies are available to address glycaemic variability in management of patients with type 2 diabetes.
- Individualising care on the basis of CGM and glycaemic variability is an important long-term objective.
REFERENCES
Present disclosure: The presenter has reported that no relationships exist relevant to the contents of this presentation.
Written by: Patrick Moore, PhD
Reviewed by: Marco Gallo, MD
